Provider and staff burnout was a hot topic in healthcare prior to COVID-19. Reports indicated emotional exhaustion and a low sense of personal fulfillment from work. This in turn makes it harder to connect with patients leading to lower patient satisfaction and poorer health outcomes. During the pandemic, this has become an even bigger topic of discussion in the healthcare industry. Employees' burnout adversely affects employees' morale resulting in low employee retention.
Identify Burnout First
Burnout impacts many organizations in the healthcare world. Burnout, according to the World Health Organization, “is a syndrome conceptualized as resulting from chronic workplace stress that has not been successfully managed. It is characterized by three dimensions: feelings of energy depletion or exhaustion; increased mental distance from one’s job, or feelings of negativism or cynicism related to one’s job; reduced professional efficacy.” We can all agree that burnout adds stress to our practices and, in addition, impacts the individuals experiencing the burnout.
Signs or symptoms to look for in your practice and individuals to identify burnout.
Not everyone experiences the same symptoms of burnout. Here, we will learn how to identify different types of symptoms related to burnout in an individual to help identify problematic areas in a practice. Some of the symptoms can be visual but some can be more subtle depending on the individual. Emotional and Physical signs can include:
- Loss of motivation
- Detachment
- Sense of failure and self-doubt
- Increasingly cynical and negative outlook
- Fatigue
- Illness
- Calling in Sick a lot
Areas in the workplace that contribute to burnout and staff satisfaction.
If you’ve noticed staff or providers showing any of the symptoms mentioned above, it might be time to evaluate one another and your practice. Some factors that can contribute to these symptoms could be related to productivity expectations, patient complexity, documenting requirements, administrative tasks, late and on-call hours, negative leadership behaviors, advancement opportunities and salary limitations. A person may also have personal characteristics that lead to burnout because they may be too self-critical, they are perfectionists, there could be a work-life imbalance, they may not have a support system outside of the office and may not have coping strategies to effectively deal with added stress.
How can you collect the information to find out if staff is experiencing burnout?
- Suggestion box
- Staff and patient surveys
- HR discussions
- Open discussion in team meetings
- Gossip chain
- Anonymously
How do you measure change after you have collected your data?
-1.png?width=153&name=Untitled%20design%20(11)-1.png)
Identify satisfaction, retention and burnout before you start to act. Then, find the key indicators of the data you collected and what will be your next action steps for the solution. When you start to assess burnout, it is important to start the action right away to reduce burnout as soon as possible. Understanding the best method to collect this data for all your employees is also essential. Some employees will be open to communication, but others may not.
Where to start eliminating burnout?
Start with your Human Resources. Build activities to assess burnout into existing HR processes. You can do this by integrating practices into your annual assessments, performance reviews (areas of strength and opportunities for improvement) and exit interviews. Continuous monitoring will help align with other HR Functions.
Define the tools for this process that you are going to use. This could be starting a peer discussion group, surveys, focus groups, written assessments or suggestion boxes.
Engagement with Senior Leadership can resolve issues rather quickly. When you engage your leadership staff and or your board, you can reveal inside knowledge to guide you through new processes.
General solutions for staff to reduce burnout and maintain staff retention.
- Identify successful interventions other healthcare practices have implemented
- Utilize team-based care model
- Assign specific administrative time for clerical tasks
- Offer flexible or part-time work schedules
- Promote shared decision making
- Train continuously
- Embrace technology
- Offer professional development opportunities
Staff surveys like the Mini Z Assessment, the Maslach Burnout Inventory and the KLAS Arch Collaborative Survey can help measure and increase employee engagement, give employees a voice, direct organizational growth and benchmark results.
What are some operational burdens identified for providers?
- Knowledge constraints
- EHR training (initial and ongoing)
- Information overload
- Alerts, summary screens, customization
- Work environment
- Work hours, schedules, panel size and acuity
- Inefficiencies of the EHR
- Use single sign on
- Consider the setting for timing out or EHR and other systems
Best practices to reduce provider burden
There are many strategies to help reduce burden for providers. To help with overall efficiency and patient visits, we have noticed artificial intelligence has come into its own. Natural Language Processing is the ability for computers to understand the latest human speech terms and text. It’s used in current technology to support spam email privacy, personal voice assistants and language translation applications. This helps computers understand and manipulate human language and can be very valuable for providers and staff.
In order entry and standing orders, there is a huge overload of information for staff and providers. It is crucial to understand what is important, what is critical to be known, what needs to be known at time of visit and what is important in visit and post visit. You can use this data during the time you have with the patient to overall have a better outcome.
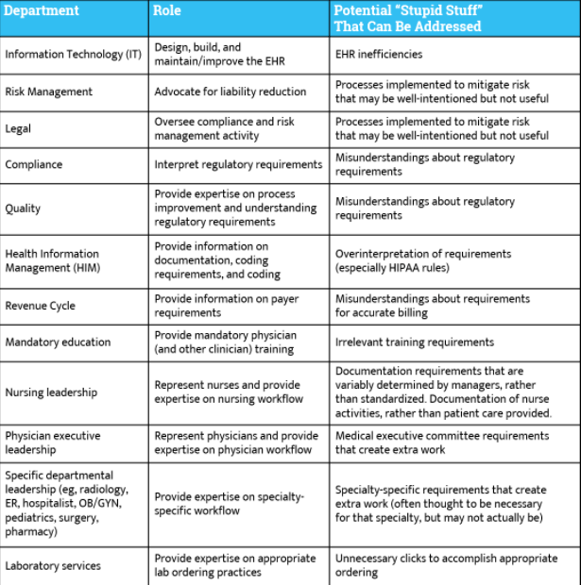
According to the American Medical Association, (AMA), “It is important to include other departments to support the initiative. By engaging common stakeholders, the initiative is set up for greater success, particularly if other departments can significantly improve their processes and work towards a common organizational goal. It is also recommended to include other departments at the beginning of your planning stages to prevent any potential barriers or delays to a solution. Please see the table below for common collaborations and how to get rid of the ‘Stupid Stuff’.”
Health IT as part of a solution
When we look at the culture of health IT, it is something that needs to have support from the executive level down. Starting at the top, your executives need to all be on the same page with the Electronic Health Record System that is currently in use.

Interoperability in relation to healthcare is defined as the ability of computer systems or software to exchange and make use of information. The exchange of information between health systems is flowing faster than ever before, and new technology innovations are bringing more usable digital health information to providers and beyond.
Not all healthcare providers can adapt at the same pace and there have been many hiccups in technology advances. Workloads have changed from a pile of charts to an inbox or a PAQ. Some of the same bad practices have been carried over from habits developed since the use of paper charts.
The Office of the National Coordinator for Health Information Technology (ONC) has developed three Burden Reduction Goals that cover various ways to reduce provider burden:
- Reduce the effort and time required to record information in EHRs for health care providers during care delivery.
- Reduce the effort and time required to meet regulatory reporting requirements for clinicians, hospitals, and health care organizations.
- Improve the functionality and intuitiveness (ease of use) of EHRs.
 The ONC released a report in February of 2019 that focuses on four key areas to help reduce burden for providers including: clinical documentation, health IT usability; federal health IT and EHR reporting requirements, and public health reporting. These areas of focus are to bring doctors back to the most important part of their profession–care for the patient–through a variety of strategies, recommendations and policy shifts.
The ONC released a report in February of 2019 that focuses on four key areas to help reduce burden for providers including: clinical documentation, health IT usability; federal health IT and EHR reporting requirements, and public health reporting. These areas of focus are to bring doctors back to the most important part of their profession–care for the patient–through a variety of strategies, recommendations and policy shifts. NextGen Configurations Opportunity:
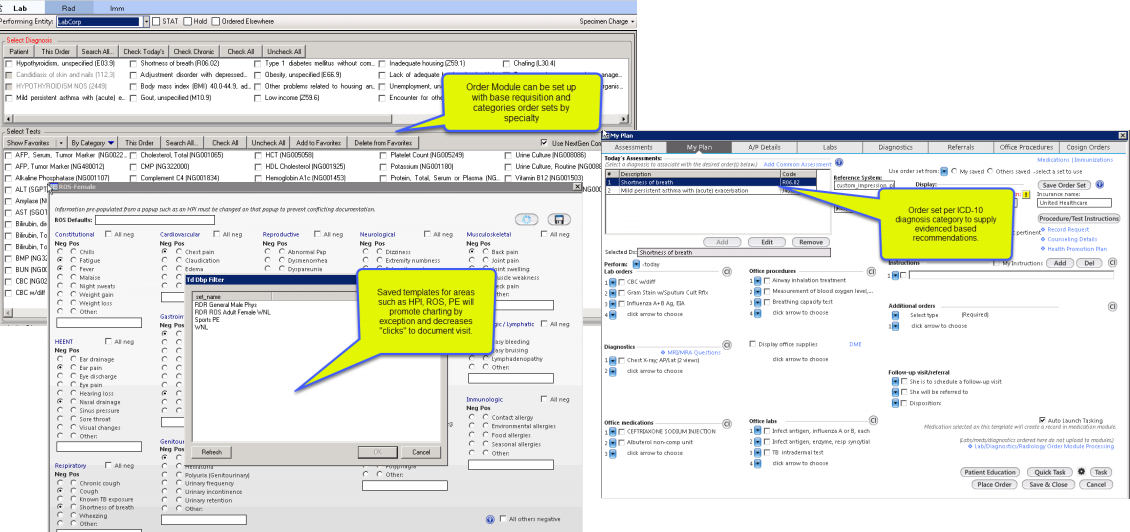
NextGen as a CERT Platform offers multiple configuration areas that promote efficiency and workflow. We usually hear from end-users that they lack the time or education to configure. Some areas are for practice implementation, while others may be specific for individual configurations. Some of the configurations that end-users may not be familiar with are:
- Order Sets
- Standing Orders
- Diagnosis based
- Provider favorites
- Lab vendors
- Saved template sets – prepopulated templates
- Individual portions: HPI, ROS, PE, etc.
- Complete visit memorized set
- Visit type configuration for workflows – framework navigation configured for practice
- Medication favorites to streamline medication scribes
- Diagnosis favorites
Here are a few examples of the NextGen Configurations that can be customized for your practice to help assist with reducing burden.
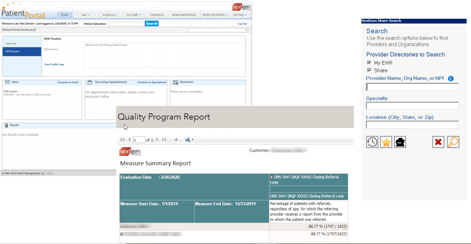
NextGen HIT Opportunities CHC’s can depend on to help reduce burden include:
- NextGen Mobile
- HQM - reporting tool
- API Interfaces
- Ryan White Reporting Console
- EDI - patient appointment reminders
- E-prescribing (ePS and ePCS)
- NG Share- send CCDA for transitions of care
- Patient Portal- patient access to health information, appointments, billing, etc. MedFusion for future
- Carequality- request and receive CCDA documents for patients
- UDSX Console- reporting tool for Uniform Data Set for HRSA
- Indian Health Services Reporting Tool
- NextGen Population Health Analytics- reporting tool with ability to interface with labs, payers, etc.
- Prescription Drug Monitoring Program (PDMP)
These are examples of how NextGen meets ONC Requirements for their Certification.
Creating a Culture of Improvement
Workforce Wellness is defined not only by the tasks being done, but by establishing a change in culture. This begins with leadership and how your organization relies on your leadership team. Create an environment where accountability is not only for your medical staff, IT staff or administrative staff, but cohesive throughout your entire practice to help reduce unnecessary stress. Create a business case to analyze the overall financial costs of your practice, including training costs, lost patient income and recruitment. This may help you understand more about patient satisfaction. If there is constant turnover and new employees are trained, patients have trouble connecting with unfamiliar staff.
To learn more about Workplace Wellness, Mental Health America conducted a two-year research project on workplace mental health with reports released in 2017 and 2019 on how the workplace affects mental health. These reports give a broad picture of what can cause workforce burnout and generate ideas on how to plan for better wellness in your practice.
Now that we have identified the symptoms of burnout, how to assess it and reduce the burden that leads to burnout, we can discuss where to start. We’ve said it previously and want to stress how important it is to involve your leadership and get the commitment from them in the initial phases of assessing burnout and developing your new plan. Rank your actions based on importance including ability to change, your resources, and the functionality of your EHR or other third-party resources. Finally, track your action plan progress. Tracking your progress enables you to evaluate your goal of creating a better workplace environment and improving patient satisfaction.
Sources: AMA Steps Forward Module, https://edhub.ama-assn.org/steps-forward/module/2757858
Mental Health America, https://www.mhanational.org/workplace-wellness
Official Website of The Office of the National Coordinator for Health Information Technology (ONC), https://www.healthit.gov/