Appropriate Use Criteria (AUC) impacts physician offices, hospital outpatient departments (including emergency departments), ambulatory surgical centers, and any other provider-led outpatient setting determined appropriate by the Secretary of Health and Human Services. In this post, we will discuss some FAQs we receive at OSIS about AUC – the clinical decision support (CDS) tool that provides advanced diagnostic test recommendations based on clinical criteria from within the patient chart. We will also review how to configure AUC within NextGen® Healthcare EHR to help implement this new workflow into your health center.
Why is AUC being implemented? This is part of the Protecting Access to Medicare Act (PAMA) established in 2014 to increase the rate of appropriate advanced diagnostic imaging services provided to Medicare beneficiaries. The original mandate has been delayed for several years, and the time has now come to formally implement. If AUC was implemented in 2020 and/or planned for implementation in 2021, this is considered an education and operations period. This grace period should allow for internal organizational set-up and workflow operations to iron out the wrinkles. Claims will not be denied during this period.
When is the new deadline? The new deadline for compliance is January 1, 2022.
What do we need to do to prepare and comply for this new deadline? To comply, additional AUC details will need to be provided to the radiology facility and must be added to advanced diagnostic service claims to avoid payment reductions, penalties, or rejections for performing entities via interface or order requisition.
These include:
- The ordering professional's NPI
- Which clinical decision support mechanism was consulted
- Whether the service ordered would or would not adhere to consulted AUC or whether consulted AUC was not applicable to the service ordered
What are the Medicare AUC scoring requirements? AUC scoring requirements are based upon payer and diagnostic study. Currently, Medicare is the only payer requiring compliance. Examples of advanced diagnostic studies include CT, PET, Nuclear Medicine, and MRI are the only categories of tests currently affected. The extent of this change only affects a limited patient population which should alleviate some angst.
Does this apply to Medicare Advantage plans too? Medicare Advantage follows guidelines of Centers for Medicare & Medicaid Services (CMS) and associate with Medicare, we recommend to include Medicare Advantage as a Payer promoting AUC.
We use NextGen, how will NextGen aid in this change? The recommendation is generated from ACR Select (a free service that has partnered with NextGen) to provide alternate tests with higher scores that providers can select and order or circumvent depending on the patient’s needs. Those on NextGen versions earlier than 5.9.2020.1 would need a patch to be applied to ensure all necessary functionality is available for regulation compliance.
Does the version of NextGen matter for System Configuration? Yes, the extent of system set up is dependent upon version of your EHR (Electronic Health Record).
What is the first step to configuring the AUC in NextGen? The first step is to ensure that your EHR contains the latest NextGen Compendium update. This can be confirmed by launching the Orders Management Console from the application launcher. If an update is available, it should be downloaded.
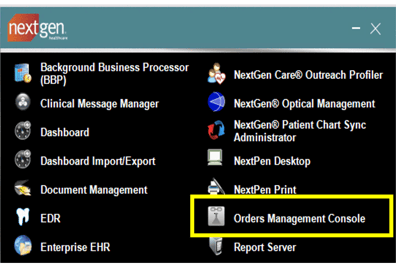
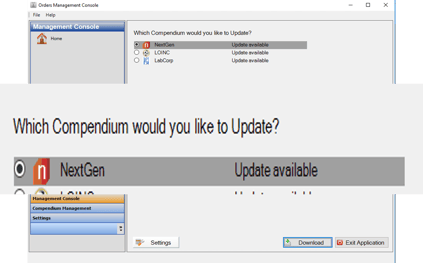
In what order should the set-up items be configured in NextGen EHR? First, check the Order Management Console to ensure the most up-to-date list of tests is in your NextGen Compendium, as shown in the above photos.
Then the remaining items in File Maintenance can be done at any interval. The majority of the set up resides within File Maintenance. All impacted radiology studies will require activation of AUC on the test compendium code.
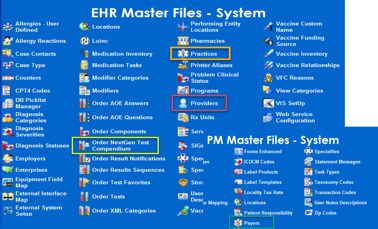
Below, we walk through the setup elements necessary to configure AUC in your NextGen experience.
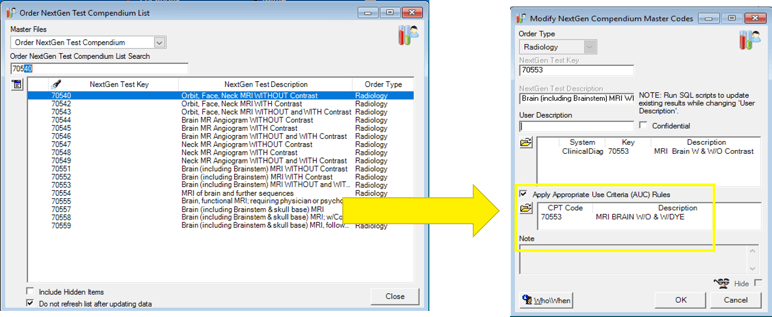
NextGen EHR version 5.9.1 and later: The download of the NextGen Compendium from Orders Management Console previously reviewed should have accomplished configuration of the most up-to-date list of tests in your NextGen Compendium. We recommend verifying some of the CT, PET, NM, and MRI orders to ensure that AUC Rules have been activated.
NextGen Version 5.9 or earlier: To set up, navigate to the Order NextGen Test Compendium table > select the test requiring AUC. The corresponding CPT code must be applied, and the Apply Appropriate Use Criteria (AUC) Rules checkbox must be selected.
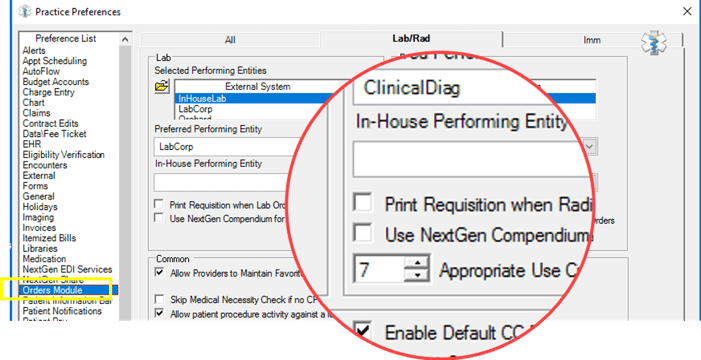
From Practice Preferences located in the Practice table > Select Orders Module > Lab/Rad tab > Confirm Appropriate Use Criteria Threshold is set as 7.
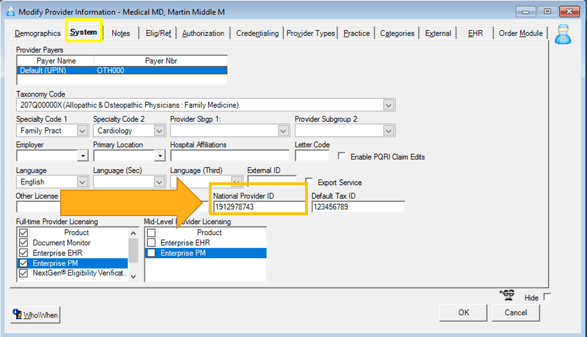
On the System tab of the Modify Provider Information template, all ordering providers must have a National Provider ID (NPI) attached to their provider profile.
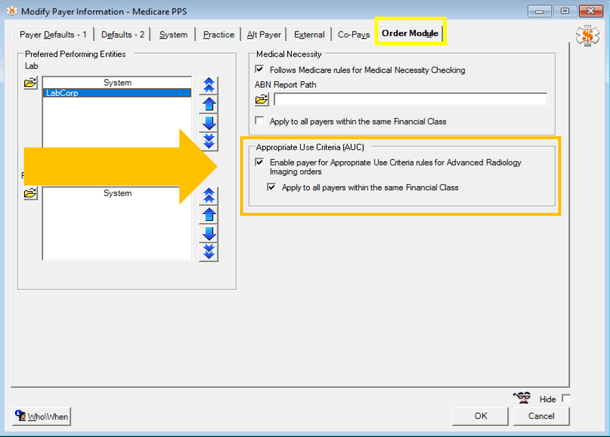
Since AUC is driven by payer, Medicare payers will require an update to the Payer Master List. In the image below, enable the payer for Appropriate Use Criteria (AUC) Rules for Advanced Radiology Imaging orders. Here, this can also be applied to all payers within the same Financial Class to eliminate the need to touch all payers.
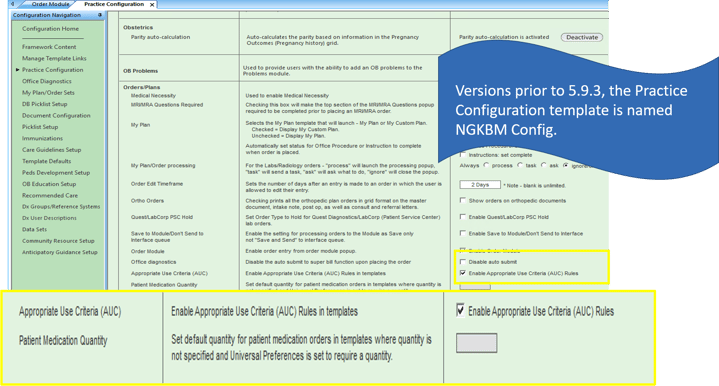
Once all File Maintenance configuration has been completed, the last step for activating AUC is from within your EHR. All other set up can be completed in preparation for implementation but this is the step that turns on the functionality.
This setting is located on the Practice template named Practice Configuration > Navigate to Orders/Plan > Enable AUC Rules.
Should we complete configuration in our test environment first? Best practices include testing in your test environment first. This will help ensure everything is working appropriately, prepare staff for the change, and highlight the containment of the setup. Take as much time as needed during the operations and test period to help.
Does IMO Procedure search impact AUC? Yes, if you have IMO Procedure Search, it does not take AUC into consideration, and bypasses the scoring system. This is currently under submission to get this corrected and workflow should be considered.
What happens if you do not enable AUC? If you do not enable AUC and are not providing the information to Diagnostic facilities, you risk the diagnostic facilities refusing to conduct those studies on your patient. AUC is impacting the revenue from the payers; the diagnostic facilities may push back and disrupt patient care. They require it and will most definitely contact the office to request the information. We highly recommend that you implement AUC to avoid any delays in patient care.
Do not wait until the deadline to implement! Take advantage of the education and operations testing period to acclimate your health center with enough time and consideration for the new workflow.
Resources:
