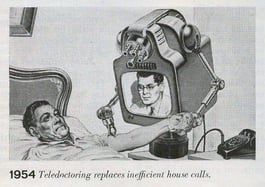
After months of treating patients through Telehealth, we now have a clearer idea of how to treat patients electronically. Given the new normal, we have learned that each patient visit is unique. Patients can be seen for symptom triage, care for chronic conditions, lab results, lifestyle management, post-operative treatments, treatment protocols, behavioral health, group education consults, after-hours care, and more. Telehealth is a bit different from the picture to the right from 1954, but as technology evolves, we’re essentially moving in that direction.
The American Medical Association (AMA), describes telehealth between patients and clinicians as:
1. Asynchronous text and photo exchanges through patient portals, health system apps, or website chat features.
2. Synchronous audio and video appointments through telehealth platforms, apps, or in-clinic technologies.
According to Dr. Sarita Nori Dermatology at Harvard Vanguard Medical Associates, “Implementing a telehealth program is a winding road at first. It takes a bit of patience and flexibility, but it’s well worth it, and the end of the road is satisfying for all involved.”

Establishing a telehealth workflow for your practice may be significant and timely, so at OSIS we have compiled a comprehensive list to advance telehealth visits for providers and care team members. Patients may initially be reluctant to schedule a telehealth visit if they are unfamiliar with the technology or fear telehealth visits lack professional standards. It is important that patients feel comforted and physicians portray the same bedside manner as an in-office visit.
The list below is not comprehensive, but rather some key considerations when preparing for telehealth visits.
First Steps:
- Sign up for a telehealth platform in order to hold online appointment
- Call your insurers to make sure you understand their reimbursement policies
- Determine what your state’s policy is on getting patient consent
- Create your office visit environment
Setting Up Your Environment:
- Ensure your setting/room is private (HIPAA)
- Address the size, location, and layout of exam room or office
- Choose a neutral background such as a gray or a light blue color
- Pay special attention to décor and furniture in the room to make sure it’s not too busy and will create a distraction for patients
- Make sure there is adequate lighting for effortless patient triage
- Avoid background noise
Equipment Set Up
- Choose what type of technology you’ll use – either desktop, tablet, or smartphone
- Have a high-speed internet connection
- Use a headset or microphone to help minimize background noise and ensure clarity
- Use dual screens if possible, for easy documentation of EHR notes
- Minimize and mute all other applications
- Make sure your software is updated
- Check that you’ve granted access to your computer’s camera and audio
- Do a trial run each day before first visit to ensure equipment is working properly
Patient Preparation
- Prepare for the patient visit as you would if the patient were in the office
- Dress with the same level of professionalism
- Review patient complaints and records before beginning the call, not during
Office Visit Communication Best Practices
- Confirm patient name and date of birth
- Adjust webcam to eye level to ensure you have eye contact with your patient
- Pause after patient speaks to allow for transmission delay
- Speak clearly and deliberately
- Choose empathetic language
- Use non-verbal language to signal that you are listening
- Verbalize and clarify next steps, such as follow-up appointments, care plan, or prescription orders
- Allow for questions from the patient and pause between questions
- Send patient survey to new patients and existing patients to improve future appointments
Each health care organization is unique and will need to consider circumstances and availability for administering their own telehealth services.
Resources: Department of Health and Human Services
American Medical Association, Telehealth Implementation Playbook
-2.png)